-
Overview
When your body is exposed to high levels of the hormone cortisol for a long time it is called Cushing syndrome. Hypercortisolism is the most common cause of Cushing syndrome. It is caused by the use of oral corticosteroid medication. The condition can also occur when your body makes too much cortisol.
An excess of cortisol can produce some of the hallmark signs of Cushing syndrome — a fatty hump between your shoulders, a rounded face, and pink or purple stretch marks on your skin. Cushing syndrome can also result in high blood pressure, bone loss and, on occasion, diabetes.
Management of Cushing syndrome can return your body’s cortisol production to normal and noticeably improve your symptoms. The earlier treatment begins, the better your chances for recovery
-
Causes
There are a number of reasons for Cushing disease and these include the following:
Pituitary adenoma – Cushing’s disease
Adenoma of the pituitary is a small, benign (non-cancerous) tumor in the pituitary. It is usually less than 1 cm in size, and is made of abnormal cells which make lots of ACTH. The ACTH stimulates the adrenals which then make too much cortisol. The abnormal cells in the adenoma are not ‘turned down’ by feedback from the high levels of cortisol.
About 4 in 5 cases of Cushing’s syndrome are caused by a pituitary adenoma if you exclude cases caused by medication (as mentioned earlier). Cushing’s syndrome caused by a pituitary adenoma is called Cushing’s disease.
Adrenal problems
Various rare disorders of the adrenal glands exist which can cause high levels of cortisol. These include:- Adrenal hyperplasia. In this disorder there is increased number and growth of the cells in the adrenal glands. These cells then make too much cortisol. There are various different types of adrenal hyperplasia.
- Non-cancerous tumor of an adrenal gland.
- Cancerous tumor of an adrenal gland (very rare).
Other causes of too much ACTH (‘ectopic ACTH’)
In many cases, some rare tumors in other parts of the body make ACTH – for example, some types of lung cancer. The ectopic ACTH (that is, ACTH not made in the pituitary) then stimulates the adrenal glands to make too much cortisol. A variety of tumors can make ACTH, some malignant, and some benign (non-cancerous). Some benign tumors are so small that it is very difficult to find where in the body the excess ACTH is being made.Steroid medicines
Steroid medications similar to cortisol are prescribed to some people to treat some disorders. This is sometimes used to treat various conditions such as some types of arthritis, and for some cancers. Long-term treatment with steroids can cause symptoms and problems similar to Cushing’s syndrome.Other causes
- People who drink too much alcohol make too much cortisol. The cortisol level goes back to normal if drinking alcohol stops.
- People with severe depression also make too much cortisol.
-
Symptoms
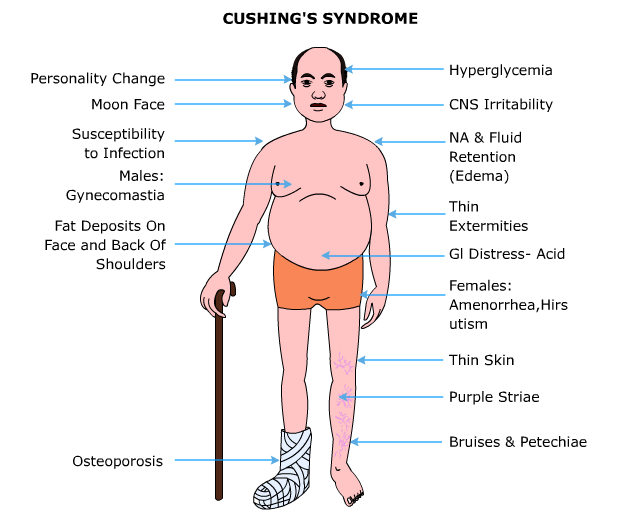
There is a variation in signs and symptoms of Cushing syndrome. Common signs and symptoms involve progressive obesity and skin changes, such as:
- Excessive gain in weight and fatty tissue deposits, particularly around the midsection and upper back, in the face (moon face), and between the shoulders (buffalo hump)
- Stretch marks that are pink or purple (striae) colored and present on the skin of the abdomen, thighs, breasts and arms
- Thinning, fragile skin that bruises easily
- Delayed healing of cuts, insect bites and infections
- Facial acne
In women with Cushing syndrome, the symptoms could include:
- Thicker or more visible body and facial hair (hirsutism)
- Irregular or absent menstrual periods
In men with Cushing syndrome, symptoms could include:
- Reduced libido
- Reduced fertility
- Erectile dysfunction
Other signs and symptoms include:
- Generalized fatigue
- Generalized muscle weakness
- Depression, anxiety and irritability
- Lack of emotional control
- Difficulties in cognition
- New or worsened high blood pressure
- Glucose intolerance that may lead to diabetes
- Headache
- Loss of bone, leading to fractures over time
-
Diagnosis
It is difficult to diagnose Cushing syndrome, particularly endogenous Cushing syndrome, because other conditions share the same signs and symptoms. It will be required to conduct a physical exam, to look for signs of Cushing syndrome. He or she may suspect Cushing syndrome if you have signs such as rounding of the face (moon face), a pad of fatty tissue between the shoulders and neck (buffalo hump), and thin skin with bruises and stretch marks.
Patients on a corticosteroid medication for a long time may be suspected of developing Cushing syndrome as a result of this medication. If you haven’t been using a corticosteroid medication, these diagnostic tests may help pinpoint the cause:
- Blood and urine tests. Doctors conduct these tests to measure hormone levels in your urine and blood and show whether your body is producing excessive cortisol. For the urine test, you may be asked to collect your urine over a 24-hour period. Both the urine and blood samples will be sent to a laboratory to be analyzed for cortisol levels.
- Other specialized tests. Tests that evaluate the blood and urine may help to determine if Cushing syndrome is present and to help identify the underlying source of any excess production. These tests often involve measuring cortisol levels before and after stimulation or suppression with other hormone medications.
- Saliva test. There is a diurnal variation associated with cortisol levels, which normally rise and fall throughout the day. In people without Cushing syndrome, levels of cortisol drop significantly in the evening. By analyzing cortisol levels from a small sample of saliva collected late at night, doctors can see if cortisol levels are too high, suggesting a diagnosis of Cushing syndrome.
- Imaging tests. Images of your pituitary and adrenal glands to detect abnormalities, such as tumors, can be provided by computerized tomography scans or magnetic resonance imaging scans.
Investigations described above help your doctor diagnose Cushing syndrome, they may also rule out medical conditions with similar signs and symptoms. For example, polycystic ovary syndrome — a hormone disorder in women with enlarged ovaries — shares some of the same signs and symptoms as Cushing has, such as excessive hair growth and irregular menstrual periods. Depression, eating disorders and alcoholism also can partially mimic Cushing syndrome.
-
Treatments
Cushing syndrome management aims to lower the high level of cortisol in your body. The best treatment for you depends on the cause of the syndrome. Treatment options include:
- Decreasing corticosteroid use. Your doctor may be able to keep your Cushing signs and symptoms under control, if they are caused by long-term use of corticosteroids, by reducing the dosage of the drug over a period of time, while still adequately managing your asthma, arthritis or other condition. For many of these medical problems, your doctor can prescribe non corticosteroid drugs, which will allow him or her to reduce the dosage or eliminate the use of corticosteroids altogether.
This reduction in dose of corticosteroid drugs should not be done on own. Do so only under your doctor’s supervision. Abruptly discontinuing these medications could lead to deficient cortisol levels. - Surgery. Your doctor may recommend complete surgical removal if the cause of Cushing syndrome is a tumor. Pituitary tumors are typically removed by a neurosurgeon, who may perform the procedure through your nose. If a tumor is present in the adrenal glands, lungs or pancreas, the surgeon can remove it through a standard operation or in some cases by using minimally invasive surgical techniques, with smaller incisions.
You’ll need to take cortisol replacement medications after the operation to provide your body with the correct amount of cortisol. You’ll eventually experience a return of normal adrenal hormone production, in most cases, and your doctor can taper off the replacement drugs. However, this process can take up to a year or longer. In some instances, people with Cushing syndrome never experience a resumption of normal adrenal function; they then need lifelong replacement therapy. - Radiation therapy. In case surgery is unable to totally remove the pituitary tumor, doctor will usually prescribe radiation therapy to be used in conjunction with the operation. Additionally, radiation may be used for people who aren’t suitable candidates for surgery. Radiation can be given in small doses over a six-week period or by a technique called stereotactic radiosurgery (Gamma Knife surgery). In the latter procedure, administered as a single treatment, a large dose of radiation is delivered to the tumor, and the radiation exposure to surrounding tissues is minimized.
- Medications. When surgery and radiation don’t work medications can be used to control cortisol production. Medications may also be used before surgery in people who have become very sick with Cushing syndrome. Doctors recommend drug therapy before surgery to improve signs and symptoms and minimize surgical risk. The tumor or its treatment will cause other hormones produced by the pituitary or adrenal gland to become deficient in some cases and your doctor will recommend hormone replacement medications. Your doctor may recommend surgical removal of your adrenal glands (bilateral adrenalectomy) if none of these treatment options is effective. This procedure will cure excess production of cortisol. Your ACTH levels, however, will remain high. This can cause excess pigmentation of your skin.
External Links/References
http://www.patient.co.uk/health/cushings-syndrome
http://familydoctor.org/familydoctor/en/diseases-conditions/cushings-syndrome.html
http://www.mayoclinic.com/health/cushings-syndrome/DS00470 - Decreasing corticosteroid use. Your doctor may be able to keep your Cushing signs and symptoms under control, if they are caused by long-term use of corticosteroids, by reducing the dosage of the drug over a period of time, while still adequately managing your asthma, arthritis or other condition. For many of these medical problems, your doctor can prescribe non corticosteroid drugs, which will allow him or her to reduce the dosage or eliminate the use of corticosteroids altogether.